Welcome to Medical Billing Knowledge-Base
In this section you can access to basics of Medical Billing , Abbreviations and terminologies used in Medical Billing, Policies, Procedures, rules & regulation and Guidlines from the key regulatory organizations of Medical Billing .
Medical Billing Process
Medical billing is the process of generating healthcare claims to submit to insurance companies for the purpose of obtaining payment for medical services rendered by providers and provider organizations. After translating a healthcare service into a billing claim, the medical biller follows the claim to ensure the organization receives reimbursement for the work the provider performed. A knowledgeable medical biller can optimize revenue performance for the physician practice or healthcare organization.
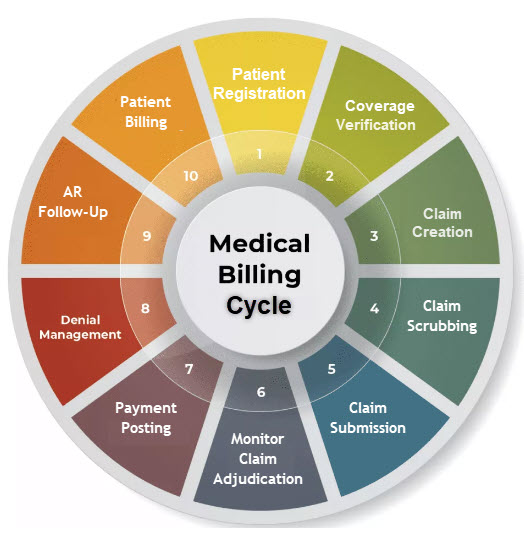
Steps of Medical Billing Process
Patient Registration-The first step is to collect patients details such as Name DOB, gender, address, and phone number. The insurance information is also collected including Insurance Name, Policy ID or number and Out of pocket information. The demographic information and insurance details must be carefully noted and should be updated. Most of the practices are using medical billing software where patient details are recoded at the first encounter and it can be used for subsequent visits.
Coverage Verification-Insurance verification is the process of contacting the insurance company through any available resource including web portals , IVR and live call to check patient eligibility whether the patent have active coverage with insurance and health insurance company covers the required procedures. This process includes deductibles, policy status, plan exclusions, and other items that affect cost and coverage and are done before patient is treated. Verifying insurance coverage and benefits ensures that services provided will be covered by the insurance.
Claim Creation-Once patient visits the provider office and received services then charges for the services rendered are entered into the Medical Billing Software in predefined format before sending it to insurance company .Claim contains CPT codes, DX codes, Modifiers, Place of service , Patient, Insurance, Provider and Facility information.
Claim Scrubbing-Before claim submission to the insurance claim is thoroughly checked to ensure it is correctly entered and coded. Insurance ,patient and provider and facility information is correct. Wrong and in valid information may result in either reduced payment or claim rejection/Denial.
Claims Submission-After Scrubbing claim next step is to submit claim to the insurance company. Claim can either be submitted electronically or paper as per insurance requirements. Most of the insurances are accepting electronic claims and a few insurances still required paper claims. Claims can be submitted directly to the insurance companies or we can use third party vendors known as clearinghouse for claim submission.
Monitor Claim Adjudication-Once claim is being submitted to insurance next step is to keep eye on the adjudication cycle. First of all claims acceptance / rejection is checked and if claim is rejected , then after removing the error claim need to be resubmitted to insurance. also one need to check claim status frequently to keep track of it.
Payment Posting-Once claim is accepted by the insurance there is no objection on claim then insurance decides to pay the claim, either in the from of a paper check or electronic fund transfer . Payments are sent along with a summary called Explanation of Benefits (EOB) and Electronic Remittance Advice (ERA). This payment need to be recorded/posted in the provider Billing software in order to keep the record and for further patient billing process.
Denial Managment-Insurance company implemented several check to validate the claim received this may include patient information verification , CPT-Dx validation , Insurance and Doctor information verification and if claim information failed through any of these checks then insurance decide to deny claim either in full or partially. Upon receiving denial notice it should be posted in system for record purpose and then necessary action need to be taken resolve the denial and resubmit claim for the reprocessing.
AR Follow-up-The Important phase of medical billing is Accounts Receivable follow-up and this is the systematic approach to track the status for unpaid claims and take action on these claim in order to resolve these claim for final processing. Several tools including clearinghouse acknowledgements , Insurance Portals, IVR , Live calls are used to track the status and then required action need to be taken according to the claim status.
Patient Billing-Once the claim has been processed by all of the insurances then patient is billed for any outstanding balances which is mainly their Co-pay, Co-insurance and deductibles. The statement which generally includes a detailed list and charges of the procedures and services provided, the amount paid by insurances and the amount due from the patient and this statement usually mailed ,emailed or faxed to the patient to received the outstanding amount. Once patient pay the amount.
Abbreviations
Below are most comman abbreviations used in Medical Billing and Coding.
Account number
This is the number assigned by provider office , Hospital or the billing software for every visit to relevent office/facility
Adjustment
The portion of charges for services rendered that provider has agreed to write off as per contractual adjustment.
Admission Date
The date on which patient got admitted to any facility for further treatment.
Advance beneficiary notice (ABN)
Notice provider gives to the patient before starting treatment informing that Medicare will not pay for the treatment or service and patient have decide whether to have the treatment and how to pay for it.
Allowed amount
insurance decides the fee for a particular service which is amount is usually less than the amount billed by the provider is called the allowed amount. Participating providers need to accept this amount while getting in contract with the insurance.
Ambulatory surgery
Outpatient surgery or surgery that does not require a saty in hospital for a night.
Ancillary service
The inpatient services patient receive beyond the room and board charges, such as laboratory tests, therapy and surgery
Appeal
This is the process by which provider can object to health plan decesion of No or less payment for care/service rendered by the provider to review and reconsider the claim.
Assignment of benefits
Agreement Patient signs to allow insurance plan to pay the provider directly for the services rendered.
Attending physician
The doctor who orders or provide the treatment is responsible for your care.
Authorization number
This is also called a Certification Number, Prior Authorization Number or Treatment Authorization Number which authorize the provider to provide specific services to patient.
Beneficiary eligibility verification
A way providers can retrieve information about whether you have insurance coverage.
Benefit contract
The legal agreement between a health plan and you. This contract establishes the full range of benefits available to you through your healthcare plan. A Benefits Contract is also sometimes referred to as a certificate of coverage or evidence of coverage.
Benefits
The extent to which your insurance coverage will pay for services provided to you. Benefits may describe what portion of the allowed amount may be due from you, the level to which they will pay for services provided by various providers, and what types of services they will or will not cover.
Bill/invoice/statement
A printed summary of your medical bill.
Brand-name drug
Drugs made and sold by a major drug company. Brand-name drugs may or may not be listed on a formulary. For any health need, there may be competing drugs from different companies. Your health plan formulary may list a specific brand-name drug if a price agreement has been made with that company. This brand-name drug will cost more than the generic version, but cost less than other brand-name drugs that are not on the formulary. If you buy brand-name drugs that are not on the formulary, you often pay more because your health plan pays more.
Certification number
A number stating that your treatment has been approved by your insurance plan. Also called an Authorization Number, Prior Authorization Number or Treatment Authorization Number.
ChampVA
Insurance linked to military service. ChampVA shares the cost of certain medically necessary procedures and supplies with eligible beneficiaries. ChampVA does not have a network of health care providers, so eligible members can visit most authorized providers.
Claim
Your medical bill that is sent to an insurance company for payment.
Claim number
A number assigned by your insurance company to an individual claim.
Centers for Medicare and Medicaid (CMS)
The federal agency that runs the Medicare program. In addition, CMS works with the states to run the Medicaid programs.
Clinical research, clinical trial or research study(Also see “Experimental or investigational treatments”)
Research conducted to evaluate the safety and/or effectiveness of a treatment, diagnostic procedure, preventive measure or similar medical intervention by testing the intervention on patients in a clinical setting. Participation in clinical research is voluntary. The informed consent form discusses who will pay the costs of services that are part of the clinical trial. Each study is different, but in many cases insurance will pay for medically necessary services that are part of the research study. Sometimes research services are paid for by the study. Check with your insurance plan or the study team to determine coverage.
CMS-1500 form
The standard paper form used by healthcare professionals and suppliers to bill insurance companies.
COBRA (Consolidated Omnibus Budget Reconciliation Act)
A federal law that protects employees and their families in certain situations by allowing them to keep their existing health insurance for a specified amount of time. COBRA provides certain former employees, retirees, spouses, former spouses and dependent children the right to temporary continuation of health coverage at group rates. The individual must pay the COBRA applies only under certain conditions, such as job loss, death, divorce or similar events. COBRA usually applies to group health plans offered by companies with more than 20 employees. premium cost to keep his/her insurance plan, but the costs are usually less expensive than individual health coverage.
Coding of claims
Translating clinical information from your medical record into numbers (such as diagnosis and procedure codes) that insurance companies use to pay claims.
Co-insurance
The amount you must pay after your insurance has paid its portion, according to your Benefit Contract. In many health plans, patients must pay for a portion of the allowed amount. For instance, if the plan pays 70% of the allowed amount, the patient pays the remaining 30%. If your plan is a preferred provider organization (see "Preferred Provider Organization (PPO)") or other narrow network type of product, your co-insurance costs may be lower if you use the services of an in-network provider on the plan’s preferred provider list. Call your insurance company for more information.
Commercial insurance plan
Commercial health insurance is typically an employer-sponsored or privately purchased insurance plan. Commercial plans are not maintained or provided by any government-run program. Commercial policies can be sold individually or as part of a group plan.
Consent for treatment
An agreement you sign that gives you permission to receive medical services or treatment from doctors or hospitals.
Co-payment (Co-pay)
A predetermined, fixed fee that you pay at the time of service. Copayment amounts vary by service and may vary depending on which provider (in-network, out-of-network, or provider type) you see. The amounts also may vary based on the type of service you are receiving (for instance, primary care vs. specialty care). For prescriptions, copayment amounts may vary depending on name-brand versus generic drugs. Call your insurance company for more information.
Coordination of benefits
How insurance companies work together when you have more than one insurance plan. A patient may be covered by more than one commercial insurance plan, such as through an employer as well as a spouse’s, parent’s or domestic partner’s employer. If you have more than one insurance plan, check with the secondary policy to find out how it covers expenses left over after your primary coverage has paid its part. (See "Secondary Insurance")
Covered benefit
Services that your insurance company pays for in full or in part.
Covered days
The days that your insurance company pays for in full or in part.
CPT(Current Procedural Terminology) code
A 5-digit numbering system that helps standardize professional and outpatient facility billing. There is a CPT code for certain types of medical services. Using this code allows healthcare providers and insurance companies to communicate and track billing more efficiently.
Date of bill
Bill preparation date. It is not the same date as the date of service.
Date of service (DOS)
Treatment date.
Deductibles
The amount a patient pays before the insurance plan pays anything. In most cases, deductibles apply per person per calendar year. With preferred provider organizations (PPOs), deductibles usually apply to all services, including lab tests, hospital stays and clinic or doctor’s office visits. Some insurance plans waive the deductible for office visits. Some plans have service-specific deductibles.
Diagnosis-related groups (DRGs)
A payment system used by many insurance companies for inpatient hospital bills. This system categorizes illnesses and medical procedures into groups. Hospitals are paid a fixed amount for each admission.
Discharge hour
The time a patient is discharged from the hospital.
Discount
The dollar amount removed from your bill, usually because of a contract between your provider and your insurance company.
Drugs/self-administered
Drugs that do not require administration from doctors or nurses. Your insurance plan may not cover these when provided as part of an outpatient service.
Due from insurance
The amount your insurance company has agreed to pay.
Due from patient
The amount you owe.
Durable medical equipment (DME)
The medical equipment that can be used many times, or special equipment ordered by your doctor, usually for use at home.
Effective date
The date on which a Benefit Contract for coverage begins.
Eligibility
A determination of whether or not a person meets the requirements to participate in the plan.
Eligible payment amount
The medical services covered by an insurance company.
Emergency care
Care provided in a hospital Emergency Department.
Emergency department
The part of a hospital that treats patients with emergency or urgent medical problems.
Estimated insurance
An estimate of payments from your insurance company.
Enrollee
A person who is covered by health insurance.
Estimated amount due
The amount the provider estimates you or your insurance company owes.
Experimental or investigational treatments(Also see “clinical research, trial or research study”)
A drug, device, diagnostic procedure, treatment, preventive measure or similar medical intervention that is not yet proven to be medically safe and/or effective. Services considered to be investigational are typically not covered by health insurance. If offered as part of a clinical research study, the study itself may cover the costs. Check with your insurance plan or study team if applicable to see if coverage is available for experimental or investigational treatments.
Explanation of benefits (EOB)
A statement sent to you by your insurance after they process a claim sent to them by a provider. The EOB lists the amount billed, the allowed amount, the amount paid to the provider and any co-payment, deductibles or coinsurance due from you. The EOB may detail the medical benefits activity of an individual or family.
Federal tax ID number
A number assigned by the federal government to doctors and hospitals for tax purposes.
Financial assistance program
Free or reduced rates for care provided to patients with demonstrated financial hardship.
Financial responsibility
The amount of your bill you have to pay.
Flexible spending account (FSA or flex account)
An employee benefit that allows a fixed amount of pre-tax wages to be set aside for qualified expenses. Qualified expenses generally include out-of-pocket medical expenses. The amount set aside must be decided in advance and employees lose any unused dollars in the account at the end of the year.
Formulary
A list of preferred prescription medicines. The formulary sorts drugs into groups, or tiers, based on how much of the costs your health plan will pay and how much you have to pay.
Generic drug
Drugs with proven benefits that cost less because they are not made by major drug companies and do not carry brand names. In almost all cases, you pay the least out of pocket for drugs in this group. Not all drugs have generic options.
Guarantor
The person responsible to pay the bill. The guarantor is always the patient unless the patient is an incapacitated adult or an unemancipated minor (under age 18), in which case, the guarantor is the patient’s parent or legal guardian.
Healthcare common procedure coding (HCPC)
A five-digit numbering system that helps standardize professional and outpatient facility billing. There is a HCPC code for certain types of medical services. Using this code allows healthcare providers and insurance companies to communicate and track billing more efficiently.
Healthcare provider
The party that provides medical services, such as hospitals, doctors or laboratories.
Health maintenance organization (HMO)
Health maintenance organization (HMO) (refers to health insurance) — These health insurance plans require enrolled patients to receive all their care from a specific group of providers (except for some emergency care). The plan may require your primary care doctor to make a referral before you can receive specialty care. An HMO may require you to live or work in its service area to be eligible for coverage. HMOs often provide integrated care and focus on prevention and wellness.
Health plan
A health plan refers to the type of health insurance you have. You may be part of a group health plan through your employer, you may have purchased an individual plan on the Health Insurance Exchange, be covered under workers’ compensation for a work-related injury, or have coverage through a government health plan such as Medicare and Medicaid.
Health savings account (HSA)
An account associated with a high deductible health plan that allows you to set aside pretax dollars to pay your deductible or other qualified medical expenses. Contributions are made into the account by the individual or the individual’s employer and are limited to a maximum amount each year. Unlike a flexible spending account, funds roll over and accumulate year after year if not spent.
HIPAA
The federal Health Insurance Portability and Accountability Act sets standards for protecting the privacy of your health information.
High deductible health plan (HDHP)
A high deductible health plan (HDHP) with a health savings account (HSA) provides medical coverage and a tax-free way to save for future medical expenses. A high deductible health plan does not usually cover healthcare costs until the deductible has been met, which means you will be responsible for healthcare costs out-of-pocket until you meet your deductible. Once the deductible has been met, eligible healthcare expenses will be covered by the plan.
Home health agency
An agency that treats patients in their homes.
Hospice
The group that offers inpatient, outpatient and home healthcare for terminally ill patients.
Hospital-based billing
This refers to the charges for services rendered in a hospital outpatient clinic or department.
Hospital charge
The amount of money the hospital charges for a particular medical service or supply.
Incremental nursing charge
The charges for nursing services added to basic room and board charges.
Individual insurance
Health insurance purchased by an individual, not as part of a group plan.
In-network
A group of doctors, hospitals and other healthcare providers preferred and contracted with your insurance company. You will receive maximum benefits if you receive care from in-network providers. Depending on your insurance plan, your benefits may be reduced or not covered at all if you receive services from providers who are not in network.
Insurance waivers
The services excluded from your insurance policy, such as cancer care or obstetric/gynecologic or pre-existing conditions.
Insured group name
The name of the group or insurance plan that insures you, usually an employer.
Insured group number
A number that your insurance company uses to identify the group under which you are insured.
Insured’s name (beneficiary)
The name of the insured person, who is also referred to as the member.
Intensive care
The medical or surgical care unit in a hospital that provides care for patients who need more care than a general medical or surgical unit can provide.
International Classification of Diseases, 10th edition (ICD-10-CM)
ICD-10-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States.
Invoice/bill/statement
A printed summary of your medical bill.
Liability
The person or persons liable or under obligation for the bill.
Lifetime maximum coverage
The Affordable Care Act prohibits health plans from putting annual or lifetime dollar limits on most benefits you receive. Plans can put an annual dollar limit and a lifetime dollar limit on spending for healthcare services that are not considered essential health benefits. The essential health benefits include at least the following:
Long-term care
The care received in a nursing home.
Managed care
A type of insurance plan that requires patients to only see providers (doctors and hospitals) that have a contract with the managed care company, except in the case of medical emergencies or urgent care, if the patient is out of the plan’s service area.
Medicaid
Medicaid is a jointly funded federal and state health insurance plan administered by states for low income adults, pregnant women, children and people with certain disabilities. For additional information, please see Your Health Insurance Coverage.
Medicare
Medicare is a federal health insurance program for people who are 65 or older, certain younger people with disabilities, and people with end-stage renal disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD). For additional information, including explanations of the different parts of Medicare, please see Your Health Insurance Coverage.
Medical record number
The number assigned by your doctor or hospital that identifies your individual medical record.
Medicare + Choice
A Medicare HMO insurance plan that pays for preventive and other types of healthcare provided by designated doctors and hospitals.
Medicare Advantage
A type of Medicare health plan offered by an insurance company that contracts with Medicare to provide you with all your Part A and Part B benefits, plus benefits that Original Medicare does not cover. For additional information, please see Your Health Insurance Coverage.
Medicare assignment
Providers who have accepted Medicare patients and agreed not to charge them more than Medicare has approved.
Medicare number
A Medicare card with a unique number is assigned to each person covered under Medicare. The number is used by providers for billing, eligibility and claim status. The Medicare Beneficiary Identifier (MBI) replaces the SSN-based Health Insurance Claim Number (HICN).
Medicare Part A
Usually referred to as Hospital Insurance, it helps pay for inpatient care in hospitals and hospices, as well as some skilled nursing costs.
Medicare Part B
Assists with paying for doctor services, outpatient care and other medical services not paid for by Medicare Part A.
Medicare summary notice (MSN)
A statement that Medicare sends to you after they process a claim from a provider for services provided to you. Also called an Explanation of Medicare Benefits (EOMB). The EOMB lists the amount billed, the allowed amount, the amount paid to the provider and any copayment, deductible or co-insurance due from you. The EOMB may detail the medical benefits activity of an individual or family.
Medicare supplements or “Medigap” policies
Policies that supplement Medicare coverage. Most times, these policies pay the Medicare co-pays and deductibles, but nothing extra. Check with your supplemental insurance to find out how it coordinates benefits with Medicare.
Network
A group of doctors, hospitals, pharmacies and other healthcare experts hired by a health plan to take care of its members.
Non-covered charges
The charges for medical services denied or excluded by your insurance. You may be billed for these charges.
Non-participating provider
A doctor, hospital or other healthcare provider that is not part of an insurance plan, doctor or hospital network.
Observation
A hospital outpatient service ordered by a physician when the physician isn’t yet sure that you will need inpatient hospital care, but feels you need outpatient monitoring at the hospital in the meantime.
Out-of-network provider
A doctor or other healthcare provider who is not part of an insurance plan, doctor or hospital network. (See "Non-participating provider")
Out of network
A doctor, hospital or other healthcare provider who is not part of an insurance plan, doctor or hospital network. (See "Non-participating provider")
Out-of-pocket costs
The costs the patient is responsible for because Medicare or other insurance does not cover them.
Out-of-pocket maximum
The most money you will have to pay before your insurance company covers all costs. Each plan sets a dollar limit for the calendar year. Once that limit is reached, the plan will pay 100% of the allowed amount for eligible charges for the rest of the calendar year. Some insurance companies do not include certain costs in this limit, such as fertility treatments or prescription drugs. Other insurance companies increase the out-of-pocket maximum for care provided by out-of-network providers.
Over-the-counter drug
Drugs that do not require a prescription. They can be bought at a pharmacy or drugstore and be dispensed to patients, while at the hospital or doctor’s office.
Paid to provider
The amount the insurance company pays to your medical provider.
Paid to you
The amount the insurance company pays to you or your guarantor.
Participating provider
A doctor or hospital that agrees to accept payment from your insurance (for covered services) as payment in full, minus your deductibles, copays and co-insurance amounts.
Patient amount due
The amount your provider charges you for services received.
Pay this amount
The amount you owe toward your medical bill.
Physician practice
A group of doctors, nurses and physician assistants who work together.
Physician practice management
Non-physician staff hired to manage the business aspect of a physician practice. The staff includes personnel from patient financial services, medical records, reception, lab and X-ray technicians, human resources and accounting.
Point of service (POS)
A type of health plan that allows members to choose to receive services from a participating or non-participating network provider. There are usually higher costs to the patient if they receive services from a non-participating provider.
Policy number
A number your insurance company gives you to identify your contract.
Power of attorney
A power of attorney is a legal document that allows you to appoint another person (called an attorney-in-fact or agent) to act on your behalf and make certain decisions for you. A power of attorney may authorize your agent to make healthcare decisions for you (when you are unable to do so), buy or sell things, manage a business, invest money, cash checks and manage your financial matters generally. Your attorney-in-fact must be over 18 years old and can be a family member, relative, or other trusted person, but cannot be your physician. You may also name multiple attorneys-in-fact in the event your primary attorney-in-fact is unable to fulfill his/her duties. Your power of attorney can be written to either take effect immediately or to take effect at some time in the future and can be written to last either for a limited period of time or indefinitely; your power of attorney ends when you die. This information is provided as a courtesy of UW Medicine. If you have any additional questions regarding powers of attorney, please seek independent legal counsel.
Pre-admission approval or certification
An agreement made by your insurance company and you or your provider, to pay their portion of your medical treatment. Providers ask your insurance company for this approval before providing your medical treatment.
Pre-existing condition
A medical condition for which the patient has received treatment during a specific period of time prior to enrolling in a new insurance plan. This period (such as 30, 60, 90 days, 6 months, etc.) before enrollment is called the “look-back” period. “Treatment” is defined as receiving medical advice, recommendations, prescription drugs, diagnosis or treatment. Under the Affordable Care Act, pre-existing condition exclusions are no longer allowed, with one exception: For individual plans (not purchased through an employer) that were in existence prior to 2010 and included such an inclusion.
Preferred provider organization (PPO)
A healthcare organization that covers a greater amount of the healthcare costs if a patient uses the services of a provider on their preferred provider list. Some PPOs require people to choose a primary care doctor who will coordinate care and arrange referrals to specialists when needed. Other PPOs allow patients to choose specialists on their own. A PPO may offer lower levels of coverage for care given by doctors and other healthcare professionals not affiliated with the PPO.
Prepayments
The money you pay before receiving medical care; also referred to as preadmission deposits.
Primary care network (PCN)
A group of doctors serving as primary care doctors.
Primary care physician (PCP)
A doctor whose practice is devoted to internal medicine, family and general practice or pediatrics. Some insurance companies also consider obstetricians or gynecologists primary care physicians.
Primary insurance company
The insurance responsible for paying your claim first, before the secondary insurance pays (for patients who are covered by more than one insurance).
Prior authorization number
A number stating that your treatment has been approved by your insurance plan. It is also referred to as an Authorization Number, Certification Number or Treatment Authorization Number.
Procedure code
A code given to medical and surgical procedures and treatments.
Prospective payment system (PPS)
A method of reimbursement in which Medicare payment is made based on a predetermined fixed amount. The payment amount for a particular service is derived based on the classification system of that service. (For example, diagnosis-related groups for inpatient hospital services.)
Provider contract discount
A part of your bill that your provider must write off because of billing agreements with your insurance company.
Provider
A hospital or physician who provides medical care to the patient.
Referral
Approval needed for care beyond that provided by your primary care doctor or hospital. For example, managed care plans (HMOs) usually require a referral from your primary care doctor to see a specialist or for special procedures.
Release of information
A signed statement from patients or guarantors that allows providers to release medical information so that insurance companies can pay claims.
Remittance advice
The explanation the hospital receives, usually with payment, from your insurance company after your medical services have been processed.
Responsible party
The person responsible for paying your hospital bill, usually referred to as the guarantor.
Revenue code
A billing code used to name a specific room, service or billing sum.
Same-Day surgery
A surgery performed as an outpatient service.
Secondary insurance
For people who are covered by more than one insurance plan, the secondary policy may cover expenses after the primary insurance has paid its part of the healthcare bill. (See “Coordination of benefits.”)
Self-insured health plan
A group health plan in which the employer assumes the risk for providing healthcare benefits to their employees. The cost for paying claims is paid by the employer.
Self-pay
A person who pays out-of-pocket for healthcare services in absence of insurance.
Service area
A geographic area where insurance plans enroll members. In an HMO, it is also the area served by your doctor network and hospitals.
Service begin date
The date your medical services or treatments began.
Service end date
The date your medical services or treatments ended.
Skilled nursing facility
An inpatient facility in which patients who do not require acute hospital care are provided with nursing care or other therapy.
Social security disability insurance (SSDI)
An income assistance program administered by the federal government for those with disabilities. The Social Security Administration (SSA) has its own definition of disability for various illnesses, such as kidney disease or diabetes. The application process can take many months. If approved, the monthly amount you receive is based on how much money you have paid into Social Security through payroll taxes. To be eligible for SSD, your disability must meet 1 of these conditions:
Have lasted or be expected to last at least 1 year.